Are you or a loved one grappling with pelvic organ prolapse (POP) and its treatment options? The FDA ban on transvaginal mesh might have left you feeling uncertain and concerned.
In April 2019, the FDA banned transvaginal mesh sales due to safety concerns, as stated by the UT Southwestern Medical Center. These products occasionally led to unsafe outcomes. In October 2022, the FDA confirmed that using surgical mesh for POP transvaginal poses more risks than benefits after a 36-month post-market surveillance study.
With transvaginal mesh no longer available, finding suitable alternatives can be overwhelming. Your well-being and peace of mind matter, and navigating this evolving landscape requires clarity and informed decision-making.
In this blog, we’ll explore the intricacies of the FDA’s transvaginal mesh ban and its impact on your journey toward managing POP.
Understanding Pelvic Organ Prolapse (POP)
POP is a common condition that primarily affects women, especially those who have gone through childbirth or reached menopause.
According to Physiopedia, it occurs when the muscles and tissues supporting the pelvic organs weaken. It causes one or more of the pelvic organs (such as the bladder, uterus, or rectum) to drop or bulge into the vaginal wall. It can lead to the following symptoms:
- Swollen vagina.
- The feeling of heaviness or pressure in the pelvis.
- Pelvic discomfort.
- Fecal incontinence, blockage, or urinary incontinence.
- Modifications to sexual function, everyday activities, and standard of living.
- Visualization of the vaginal prolapse.
- Bleeding due to the vaginal mucosa eroding.
- Constipation.
Various factors contribute to the development of POP, including childbirth, aging, obesity, chronic coughing, and connective tissue disorders. While not life-threatening, this condition can significantly impact a woman’s quality of life, causing physical discomfort and emotional distress.
Also Read N: Exploring Retail and Wholesale Investment Opportunities
Transvaginal Mesh and Its Use in POP Treatment
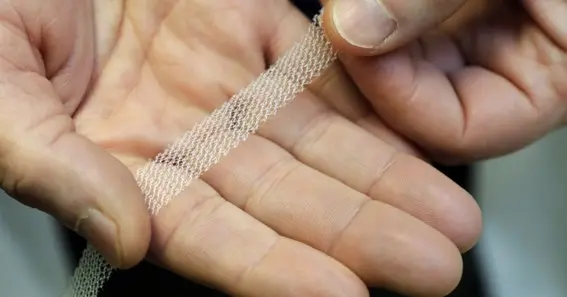
Transvaginal mesh has been widely used in treating POP to support weakened pelvic tissues and organs. It’s a synthetic surgical mesh implanted through the vagina to reinforce the pelvic floor and address the structural deficiencies contributing to the condition. Initially touted as a breakthrough solution, its popularity surged due to its minimally invasive nature and perceived effectiveness.
However, concerns regarding the safety and efficacy of transvaginal mesh have emerged. According to TorHoerman Law, numerous reports of severe complications associated with the implants have surfaced. These complications include mesh erosion, infection, chronic pain, urinary problems, and painful sexual intercourse. As a result, many women have experienced significant physical and emotional distress, leading to a decline in their quality of life.
The prevalence of complications linked to transvaginal mesh has prompted a wave of litigation against the manufacturers. As a result, has led to the emergence of the vaginal mesh lawsuit filed by affected individuals seeking compensation for their injuries and damages. The plaintiffs claim that the product makers supplied false information about the efficacy and safety of the devices.
The legal landscape surrounding the mesh has underscored the need to thoroughly evaluate its risks and benefits. It also underscores the need for informed decision-making regarding POP treatment options. Patients should consult with their healthcare providers to explore alternative treatments and make informed choices tailored to their needs and circumstances.
Also Read P: The Art of Perfecting Your Bowling Game: Strategies, Techniques, and Essential Gear
Implications of the FDA’s Ban for Patients
The FDA’s ban on transvaginal mesh for POP treatment carries significant implications for affected patients. Firstly, it necessitates reevaluating treatment options, as the device was once a commonly utilized approach for managing it. Patients may experience uncertainty and concern about finding an alternative treatment that is both effective and safe.
The ban underscores the importance of patient-provider communication and shared decision-making in healthcare. Patients need to have open discussions with their healthcare providers about their symptoms, concerns, and treatment preferences. This collaborative approach can help ensure patients receive personalized care tailored to their needs and circumstances.
The good news is that safe surgical alternate procedures are available, even after the FDA banned the mesh for prolapse repairs. As effective hammocks wrap around the urethra, alternatives such as vaginal or bladder slings, recommended by professionals, stop urine leaks during stressful situations. Tissue-based or inserting mesh strips via tiny incisions is the procedure for laparoscopic/robotic or abdominal prolapse correction, which the FDA deems safe.
Instead of utilizing synthetic mesh to rebuild pelvic organ support, transvaginal prolapse repair utilizing native tissue can be used. In this method, the patient’s tissue is being employed, minimizing risks. Regarding POP and incontinence issues, these choices provide respectable substitutes, states UT Southwestern Medical Center.
Healthcare Provider Perspective
From the healthcare provider’s standpoint, the FDA’s ban on transvaginal mesh prompts a reevaluation of treatment strategies for POP patients. The device was once a commonly used option for its repair due to its perceived benefits. That included minimally invasive placement and potential long-term support. Its associated risks have led to a shift in practice.
Healthcare providers now face the challenge of guiding patients through this transition period. They are helping them understand the implications of the FDA’s decision and exploring other treatment options. It involves engaging in open and transparent discussions with patients about their symptoms, concerns, and treatment preferences.
It also requires staying informed about the preventive strategies that can be discussed with the healthcare provider, states WebMD. For instance, kegel exercises are an effective way to develop the pelvic muscles while sustaining a healthy lifestyle to prevent POP. Constipation lessens the tension on the pelvic muscles, and maintaining a high-fiber diet, staying hydrated, and managing weight all help lower risks.
Prevent extra strain by using your legs rather than your back or abs when lifting. It’s critical to stop smoking since it raises the chance of POP. Also, it’s critical to take care of enduring health problems like chronic coughing to prevent making the disease worse. These preventative steps are intended to reduce the risk factors for pelvic organ prolapse and strengthen the pelvic muscles.
Patient Advocacy and Support
In the wake of the FDA’s ban, patient advocacy and support play crucial roles in helping individuals navigate this challenging landscape. Advocacy groups and support networks can provide a valuable source of information and guidance. They can also provide emotional support for patients grappling with the implications of the FDA’s decision.
These organizations offer platforms for patients to share their experiences, voice their concerns, and connect with others facing similar challenges. By fostering a sense of community and solidarity, patient advocacy groups empower individuals to become active participants in their healthcare journey.
Patient advocacy efforts can contribute to broader initiatives aimed at raising awareness about POP. It can advocate for improved access to alternative treatment options and promote patient-centered care.
Looking Ahead: Future of POP Treatment
The FDA’s ban on transvaginal mesh has prompted a shift in focus towards the future of POP treatment. While this decision poses immediate challenges for patients and healthcare providers, it also opens the door to innovation and advancement in its management. Researchers and medical professionals are actively exploring alternative treatment modalities that offer safe and effective solutions for patients.
One promising avenue of research involves the development of biocompatible materials and surgical techniques. These aim to provide durable support for the pelvic organs without the associated risks of mesh implantation. Also, there is growing interest in non-surgical approaches, such as physical therapy, exercises, and lifestyle modifications. These may offer viable options for symptom management and prevention of POP progression.
In conclusion, the FDA’s ban on transvaginal mesh presents a significant turning point in the treatment journey of POP patients. While it brings challenges and uncertainties, it also sparks innovation and a renewed focus on patient safety and well-being. Patients must stay informed, engage in open dialogue with healthcare providers, seek support from advocacy networks, and explore alternative treatment options.